Dental Implant Failure Prevention Guide
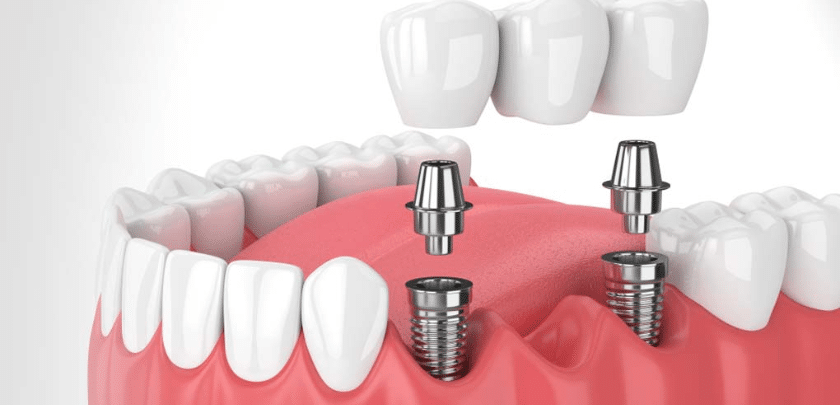
Dental implants have revolutionized the field of dentistry, offering a durable and natural-looking solution for tooth replacement. While dental implants have a high success rate, occasional failures can occur, leading to complications and patient dissatisfaction. To mitigate the risk of implant failure, it’s crucial to understand the factors that contribute to it and implement preventive strategies. In this comprehensive guide, we’ll explore the causes of dental implant failure and provide actionable tips for prevention.
Understanding Dental Implant Failure
Dental implant failure refers to the loss of integration between the implant and the surrounding bone, resulting in instability, discomfort, and potential implant removal. Implant failure can occur at various stages of treatment, including during surgery, osseointegration, or after restoration. Several factors contribute to implant failure, including:
- Poor Bone Quality: Inadequate bone quantity or density at the implant site can compromise implant stability and integration, leading to failure over time.
- Infection and Peri-implantitis: Bacterial infection around the implant site, known as peri-implantitis, can cause inflammation, bone loss, and implant failure if left untreated.
- Implant Overloading: Excessive forces applied to the implant, such as from bruxism (teeth grinding), chewing on hard foods, or improper occlusal forces, can lead to mechanical failure and implant loosening.
- Smoking and Tobacco Use: Tobacco use can impair blood flow and hinder the body’s ability to heal, increasing the risk of implant failure and complications.
- Poor Oral Hygiene: Inadequate oral hygiene practices, such as irregular brushing, flossing, and dental visits, can contribute to bacterial buildup and peri-implantitis, leading to implant failure.
Preventive Strategies for Dental Implant Failure
To minimize the risk of dental implant failure and enhance long-term success, patients and dental professionals can implement the following preventive strategies:
- Comprehensive Evaluation: Conduct a thorough evaluation of the patient’s medical history, oral health status, and bone quality using imaging techniques such as CBCT scans to identify potential risk factors for implant failure.
- Optimal Treatment Planning: Develop a customized treatment plan that considers the patient’s unique anatomical features, oral health needs, and esthetic goals. This may involve bone grafting procedures to enhance bone volume and quality at the implant site.
- Implant Site Preparation: Ensure proper implant site preparation, including adequate bone density and primary stability, to promote successful osseointegration and long-term implant stability.
- Strict Aseptic Technique: Adhere to strict infection control protocols during implant surgery to minimize the risk of bacterial contamination and peri-implantitis. Use sterile instruments, surgical drapes, and antimicrobial mouth rinses to create a sterile surgical field.
- Patient Education: Educate patients about the importance of maintaining good oral hygiene practices, quitting smoking, and attending regular dental check-ups to prevent peri-implantitis and implant failure.
- Occlusal Analysis: Perform a comprehensive occlusal analysis to ensure proper implant positioning, occlusal stability, and distribution of forces. Adjust occlusal contacts as needed to prevent implant overloading and mechanical failure.
- Prophylactic Antibiotics: Consider prescribing prophylactic antibiotics before implant surgery for patients at high risk of infection, such as those with a history of periodontal disease or systemic conditions that compromise immune function.
- Long-Term Maintenance: Emphasize the importance of long-term maintenance and follow-up care to monitor implant stability, peri-implant health, and oral hygiene status. Schedule regular recall appointments for professional cleanings, examinations, and radiographic evaluations.
- Multidisciplinary Collaboration: Foster collaboration between dental specialists, including periodontists, oral surgeons, prosthodontists, and dental hygienists, to provide comprehensive care and address complex cases of implant failure.
Conclusion
Preventing dental implant failure requires a proactive approach that addresses patient-specific risk factors, adheres to best practices in implant dentistry, and emphasizes long-term maintenance and follow-up care. By implementing comprehensive treatment planning, strict infection control measures, patient education, and interdisciplinary collaboration, dental professionals can optimize implant success rates and enhance patient outcomes. With proper care and preventive strategies, dental implants can continue to serve as a reliable and predictable solution for tooth replacement, restoring function, esthetics, and quality of life for patients worldwide.